Shoulder
Shoulder Arthritis
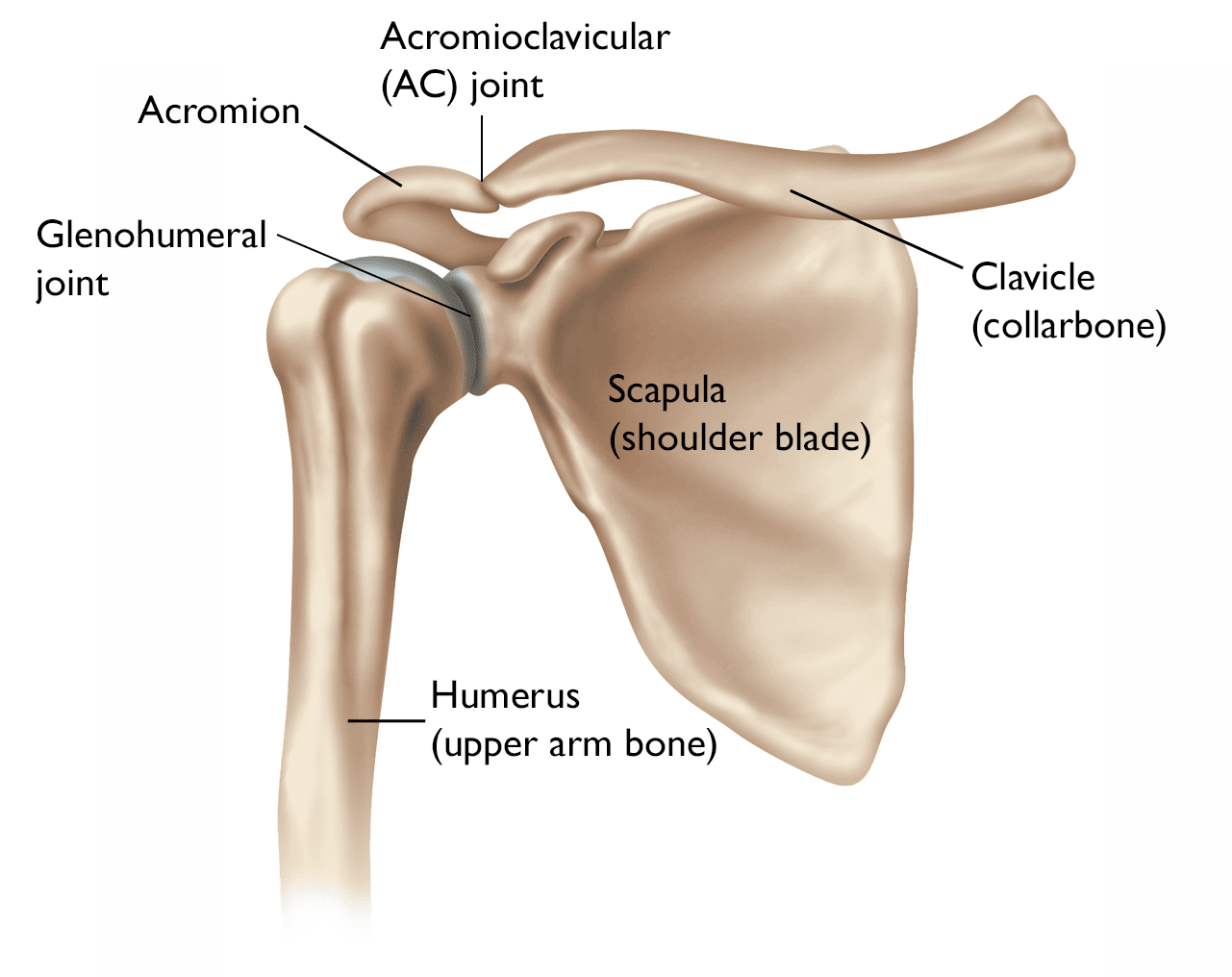
Shoulder arthritis is a condition where the cartilage in the shoulder joint deteriorates, leading to pain, stiffness, and limited movement. The shoulder joint, formed by the upper arm bone (humerus), shoulder blade (scapula), and collarbone (clavicle), is highly flexible, which allows for a wide range of motion. Arthritis in this joint can significantly impact a person’s ability to perform daily activities and engage in physical activity.
Types of Shoulder Arthritis
There are two main types of arthritis that can affect the shoulder joint:
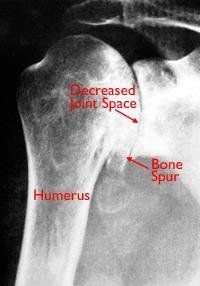
- Osteoarthritis (OA): This is the most common form of shoulder arthritis, typically associated with aging. It occurs when the cartilage that cushions the bones in the shoulder wears down over time, causing the bones to rub against each other, which leads to pain, stiffness, and swelling.
- Rheumatoid Arthritis (RA): This is an autoimmune condition where the body’s immune system mistakenly attacks the synovial lining of the joints, including the shoulder. This results in inflammation, pain, and damage to the cartilage and ligaments around the shoulder joint.
Symptoms of Shoulder Arthritis
The symptoms of shoulder arthritis can vary depending on the severity of the condition and the type of arthritis. Common symptoms include:
- Pain in the shoulder, particularly with activity or after long periods of use
- Stiffness that may make it difficult to move the shoulder or raise the arm
- Swelling in the joint
- Decreased range of motion in the shoulder, making daily activities like reaching or lifting difficult
- Pain in the shoulder blade or upper arm, especially with overhead movements
As arthritis progresses, the pain may become more constant, even interfering with sleep or routine activities.
Causes and Risk Factors
The causes of shoulder arthritis can vary based on the type of arthritis:
- Osteoarthritis often develops due to years of wear and tear on the joint. It can be exacerbated by excessive strain, past injuries, or genetic predisposition. Age is the biggest risk factor, with arthritis becoming more common as individuals age.
- Rheumatoid arthritis is an autoimmune disorder, where the body attacks the synovium in the shoulder joint, leading to inflammation and joint degradation. Genetic factors, infections, and environmental factors can trigger RA in susceptible individuals.
Other risk factors for developing shoulder arthritis include:
- Previous shoulder injuries, such as fractures or rotator cuff tears
- Inflammatory conditions, including gout or lupus
- Genetics, with a family history of arthritis increasing the likelihood of developing the condition
- Obesity, which can increase the load on the joints, accelerating wear and tear
Diagnosis of Shoulder Arthritis
The diagnosis of shoulder arthritis involves a thorough physical examination and review of medical history. Dr. Ryan du Sart will assess the joint’s range of motion, check for tenderness, and look for any deformities. Imaging tests are essential in confirming the diagnosis and determining the extent of cartilage damage. Common imaging techniques include:
- X-rays: These are used to evaluate bone changes and joint space narrowing that are typical of arthritis.
- MRI: In some cases, an MRI may be used to assess the soft tissue around the joint, including the cartilage and muscles.
- CT scans: These can be used if more detailed images are needed, especially if there are concerns about bone spurs or fractures.
Treatment Options for Shoulder Arthritis
Although shoulder arthritis cannot be cured, treatment options can help manage symptoms, reduce pain, and improve function. The treatment plan will depend on the type of arthritis and the severity of the condition.
Non-Surgical Treatment
In the early stages of arthritis, conservative treatments can be effective in managing symptoms:
- Pain relief: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or paracetamol can help manage pain and reduce inflammation.
- Physical therapy: Targeted exercises can improve strength, flexibility, and range of motion in the shoulder. A physiotherapist will provide specific exercises to help restore function.
- Steroid injections: Corticosteroid injections can provide temporary relief by reducing inflammation in the shoulder joint.
- Activity modification: Limiting activities that exacerbate pain, such as overhead movements or heavy lifting, can help reduce stress on the shoulder.
Surgical Treatment
When non-surgical treatments are no longer effective, surgery may be recommended. Surgical options vary depending on the severity of the arthritis and the impact on daily life.
- Shoulder Arthroscopy: In some cases, arthroscopy can be used to clean out the joint, remove bone spurs, and smooth the joint surfaces to reduce pain and improve mobility. However, this procedure is generally more effective for individuals with less advanced arthritis.
- Total Shoulder Replacement (TSR): For more advanced arthritis, a total shoulder replacement may be necessary. This involves removing the damaged parts of the shoulder joint (the humeral head and glenoid) and replacing them with prosthetic components. This surgery can relieve pain and restore function, particularly for patients with severe arthritis.
- Reverse Total Shoulder Replacement: In cases where the rotator cuff is severely damaged or torn (rotator cuff tear arthropathy), a reverse shoulder replacement may be performed. In this procedure, the socket and ball are reversed to allow other muscles to move the arm, instead of relying on the rotator cuff.
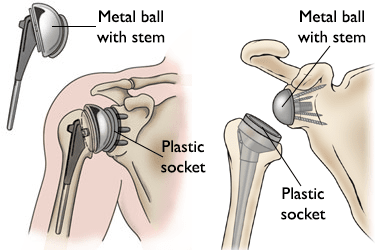
Recovery and Rehabilitation
Recovery from shoulder arthritis surgery will vary depending on the procedure and the individual. After a shoulder replacement, patients will typically need to undergo physical therapy to regain strength, improve range of motion, and restore function. This process can take several months, with a return to normal activities typically occurring within 6-12 months, depending on the individual’s progress.
Postoperative care generally includes:
- Pain management: Regular use of pain medications, such as paracetamol or NSAIDs, may be required in the first few weeks following surgery.
- Physical therapy: Rehabilitation is essential to regain function and mobility in the shoulder joint. Exercises will be prescribed to improve strength and movement.
- Gradual return to activity: Patients will be encouraged to gradually return to daily activities, with high-impact activities being avoided for several months.
Preventing Shoulder Arthritis Progression
While you cannot reverse arthritis, you can take steps to prevent it from progressing:
- Maintaining a healthy weight: Reducing the load on the shoulder joints can help slow the progression of arthritis.
- Regular exercise: Low-impact activities like swimming, cycling, and walking can help strengthen muscles around the shoulder and reduce strain on the joint.
- Avoiding excessive strain: Protecting the shoulder from repetitive overhead activities or heavy lifting can reduce wear and tear on the joint.
Why Choose Dr. Ryan du Sart?
Dr. Ryan du Sart is an experienced orthopaedic surgeon specialising in shoulder arthritis and joint replacement procedures. With his patient-centred approach, Dr. du Sart offers tailored treatment plans designed to improve quality of life and restore function for individuals with shoulder arthritis.
Book a Consultation
If you are experiencing shoulder pain or think you may have arthritis, don’t wait. Early diagnosis and intervention can help reduce symptoms and slow the progression of the disease. Contact Dr. Ryan du Sart’s office today to schedule your consultation.
Phone: (08) 9779 9767
Email:
admin@ryandusart.com.au
Clinic Locations:
6 Higgins Street, South Bunbury, WA 6230
20 Prince Street, Busselton, WA 6280
References:
- Felson, D. T., et al. (2015). "Osteoarthritis: A review of the epidemiology, diagnosis, and management." American Family Physician.
- Smith, T. O., et al. (2014). "The effectiveness of shoulder arthroplasty for osteoarthritis: A systematic review of the evidence." Bone & Joint Journal.
- Jana, S. et al. (2016). "Rheumatoid arthritis: Clinical findings, diagnosis, and management strategies." Journal of Clinical Orthopaedics.
- Kreder, H. J., et al. (2020). "Total shoulder arthroplasty: Current indications, techniques, and outcomes." Orthopaedic Clinics of North America.

