Foot & Ankle
Achilles Tendinitis
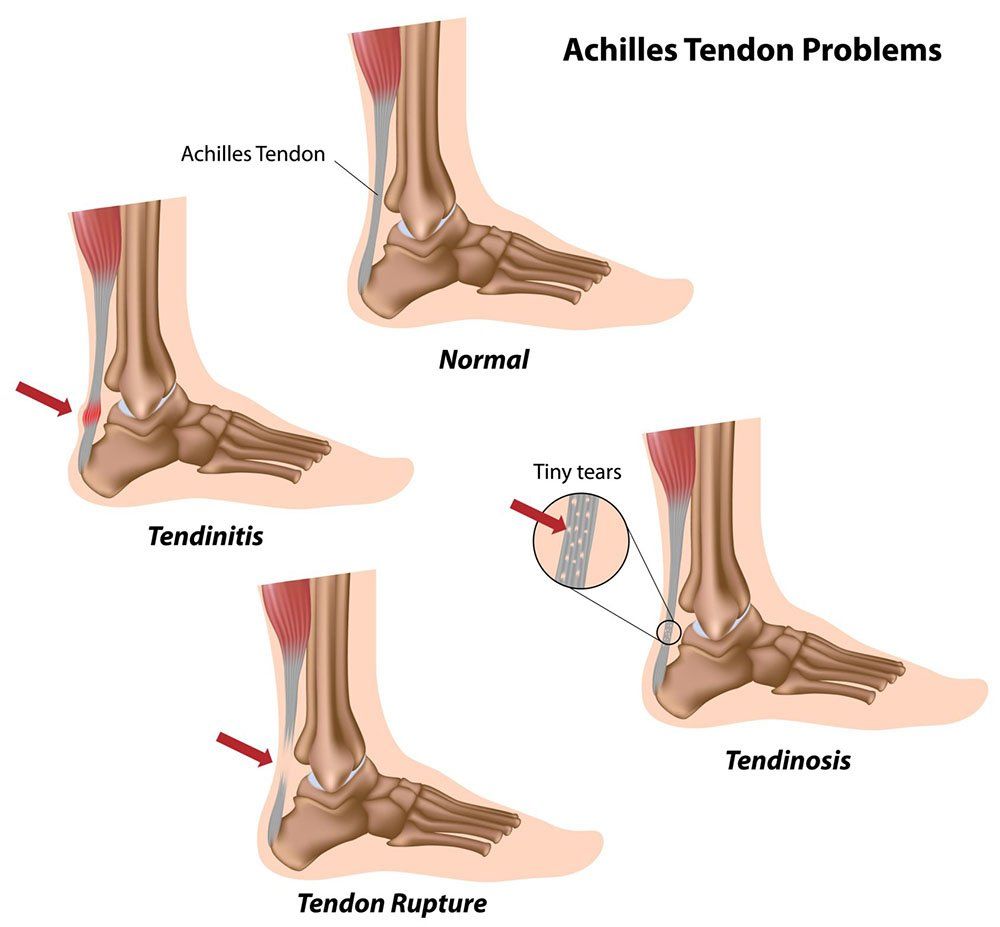
Achilles tendinitis is a common condition that involves the inflammation or injury of the Achilles tendon, which connects the calf muscles to the heel bone. The Achilles tendon is one of the largest and most important tendons in the body, as it plays a critical role in activities such as walking, running, and jumping. Achilles tendinitis can result in significant pain and restricted movement, making it difficult for individuals to participate in physical activities.
Achilles tendinitis can occur in two forms: non-insertional and insertional. Non-insertional tendinitis affects the tendon itself, causing inflammation in the middle portion. Insertional tendinitis occurs where the tendon attaches to the heel bone, often resulting in more severe pain and complications.
Symptoms of Achilles Tendinitis
The symptoms of Achilles tendinitis vary depending on the severity and type of injury. Common signs include:
- Pain and stiffness along the Achilles tendon, particularly in the morning or after periods of rest.
- Pain that worsens with activity, such as walking, running, or climbing stairs.
- Swelling and tenderness around the Achilles tendon, often accompanied by redness and warmth.
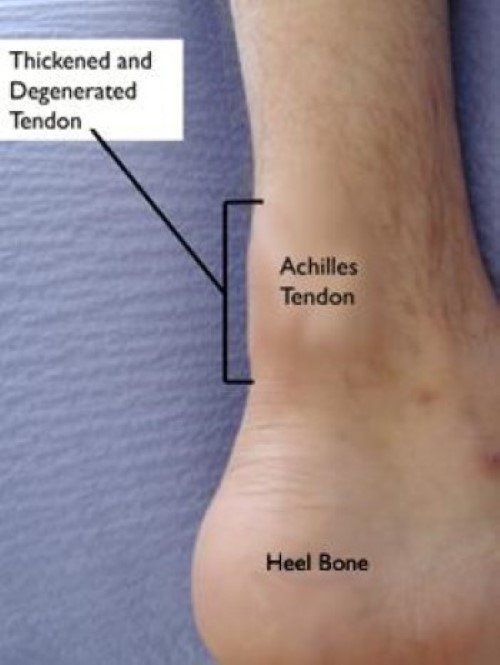
- Thickening of the tendon in more advanced cases, indicating inflammation and degeneration.
- Pain in the heel or along the back of the lower leg.
- Difficulty walking or standing for extended periods due to pain and restricted movement.

Treatment Options for Achilles Tendinitis
Treatment for Achilles tendinitis generally involves a combination of non-surgical and surgical options, depending on the severity of the injury. The primary goals are to reduce pain, promote healing, and restore mobility to the affected tendon.
Non-Surgical Treatment
In most cases, Achilles tendinitis can be treated without surgery. Initial treatment options include:
- Rest: Resting the affected leg to prevent further strain on the tendon.
- Ice therapy: Applying ice packs to the tendon for 20-30 minutes, 3-4 times a day, to reduce swelling and inflammation.
- Anti-inflammatory medications: Over-the-counter medications such as paracetamol or ibuprofen can help alleviate pain and reduce inflammation.
- Heel lifts and orthotics: Wearing cushioned heel lifts or custom orthotics reduces pressure on the tendon during walking and standing.
- Stretching and strengthening exercises: A structured physiotherapy program designed to improve the flexibility and strength of the calf muscles and Achilles tendon. Exercises can help restore motion and reduce stiffness.
- Corticosteroid injections: In cases of severe pain, a corticosteroid injection may be recommended to reduce inflammation (though not typically used for long-term treatment).
- Night splints: A night splint that keeps the foot dorsiflexed can help stretch the tendon while sleeping, improving flexibility over time.
Surgical Treatment
If non-surgical treatments fail to relieve symptoms or if the tendon is severely torn, surgery may be recommended. Surgical options include:
- Debridement (tendon cleaning): Removal of damaged tissue from the tendon to promote healing and reduce pain.
- Tendon repair: In cases of tendon rupture or severe degeneration, the tendon may be surgically repaired by reattaching it to the heel bone or removing damaged portions.
- Tendon transfer: In cases of extensive tendon damage, a tendon from another part of the foot or leg may be used to replace the damaged Achilles tendon.
- Achilles tendon lengthening: In some cases, the tendon may need to be lengthened to reduce tension and facilitate proper healing.
Recovery and Rehabilitation
Recovery from Achilles tendinitis surgery can take several months, with rehabilitation being key to restoring mobility and strength. Post-operative recovery generally involves the following stages:
- Rest and Immobilisation: Initially, the foot will be immobilised in a cast or boot to allow the tendon to heal.
- Gradual Weight-Bearing: After the initial recovery period, patients will gradually increase weight-bearing on the affected foot, starting with crutches and moving to a walking boot.
- Physical Therapy: A customised physical therapy program will help restore strength, flexibility, and range of motion to the Achilles tendon.
- Gradual Return to Activity: Depending on the severity of the injury, return to high-impact activities such as running or jumping may take several months.
When to Seek Help for Achilles Tendinitis
If you are experiencing persistent pain, swelling, or difficulty moving the affected foot or ankle, it’s important to seek medical advice. Early diagnosis and treatment can prevent the condition from worsening and help avoid long-term damage to the Achilles tendon
Why Choose Dr. Ryan du Sart for Achilles Tendinitis Treatment?
Dr. Ryan du Sart is a highly experienced orthopaedic surgeon who specialises in the treatment of tendon injuries, including Achilles tendinitis. With his patient-centred approach and extensive expertise in both non-surgical and surgical interventions, Dr. du Sart offers personalised care to help restore function and relieve pain.
Dr. du Sart uses the latest techniques in tendon repair and rehabilitation to ensure the best possible outcomes for his patients.
Book a Consultation
If you are experiencing Achilles tendon pain or symptoms of tendinitis, don't wait to seek treatment. Early diagnosis and intervention can help you avoid complications and return to normal activity sooner.
Phone: (08) 9779 9767
Email: admin@ryandusart.com.au
Locations:
6 Higgins Street, South Bunbury, WA 6230
20 Prince Street, Busselton, WA 6280
References:
- Maffulli, N., & Longo, U. G. (2008). Achilles Tendinopathy: A Review of the Literature. British Journal of Sports Medicine, 42(5), 232-237.
- Khan, K. M., et al. (2003). Achilles Tendinopathy: A Review of Management. Journal of Orthopaedic & Sports Physical Therapy, 33(10), 619-632.
- Rees, J. D., et al. (2009). Achilles Tendon Pathology: A Review of Current Clinical Treatments. The British Journal of Sports Medicine, 43(3), 214-221.

