KNEE
Knee Osteoarthritis
The knee is a hinge joint made up of three bones: femur (thigh), tibia (shin) and patella (knee cap) which allows the knee to bend.
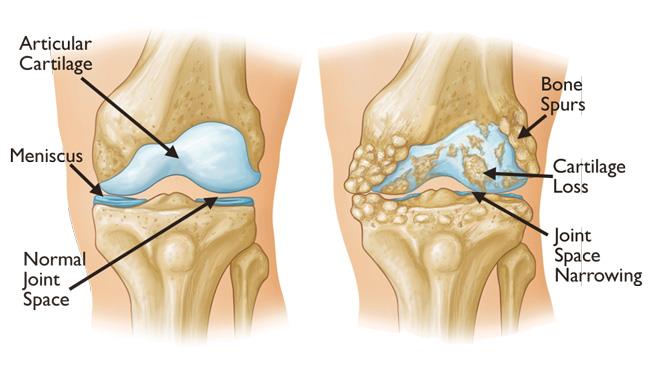
In a healthy knee, each of these bones is lined with cartilage which acts like a cushion and smooth surface allowing easy, frictionless movement. Degeneration of cartilage in the knee means there is no layer to act as a shock absorber or reduce friction. It also alters the bony surfaces and ligaments in the knee causing pain, joint stiffness and inflammation.
Symptoms
The most common symptom of knee osteoarthritis in pain. More than 50% of people over 65 years will have evidence of arthritis on an X-ray, and approximately 1 in 7 of these patients will have symptoms (1, 2). Initially pain may be only felt when doing more strenuous exercise or after prolonged periods of being on your feet. As osteoarthritis progresses, pain may be present for most of the day and even cause disruption to sleep. Depending on the location of your osteoarthritis, your symptoms will vary. Usually osteoarthritis on the end of your bones will lead to difficulty walking long distances, whereas under the kneecap you may experience difficulty and pain climbing stairs or rising from a chair.
Other symptoms individuals may experience include:
- Knee stiffness, which can be worse after a period of inactivity e.g. in the morning
- Swelling and inflammation
- Muscle weakness and joint instability
- The feeling of the knee feeling stuck in certain positions or ‘giving way’
Causes
Most common in older patients, the exact cause of osteoarthritis is not always known. It is usually slow and characterised by progressive wear and tear of the joint. Some causes of arthritis include:
- Advancing age
- Congenital or developmental knee diseases
- Weight issues
- Previous knee injury or fracture
- Increased stress on the knee due to overuse.
Diagnosis
Diagnosis is made by medical consultation and examination, taking the patient's past medical history and confirmed by X-ray of the knee. Sometimes an MRI scan may be offered, this can help determine whether pain is being impacted by other areas of the hip.

Treatment Options
Unfortunately, once damage has been done to the cartilage and tissues of the knee joint, it is irreversible and there is no ‘cure’ for osteoarthritis. Rather it is about managing your symptoms in the initial stages and progressing to more definitive treatment as your symptoms progress and as dictated by medical professionals.
Non Operative Treatment
In the early stages of osteoarthritis your GP or medical physician will probably start you on the most common non-operative treatment including pain killers (paracetomol or panadol osteo) and anti-inflammatories if tolerated and not contraindicated. It can also be helpful to manage your osteoarthritis by activity modification ie. limiting the time you are on your feet. Regularly partaking in low impact exercise (swimming, cycling, pilates, gym, yoga etc.) instead of high impact activities (running, jumping etc.) is also helpful to reduce stress on the knee joint whilst strengthening surrounding muscles.
Consulting a physiotherapist can also be beneficial for specific exercises to help increase range of motion, flexibility and strengthen the muscles in the knee.
Injections can sometimes be helpful to reduce pain if surgery is not indicated.
Three to four times your body weight is transferred through the knee joint with every step. One of the easiest ways to reduce this force on your knee is maintaining a healthy body weight by ensuring a balanced diet and regularly exercising.
Surgery
Following consultation and review, if osteoarthritis has progressed and other interventions have not succeeded, surgical intervention for treatment may be recommended. As with all surgeries, it comes with some risks and should be left as a last resort.
Total Knee Replacement
This is the most common treatment for knee osteoarthritis. It is where the damaged and diseased portions of the bone and cartilage are surgically removed and replaced. A new prosthesis made from metal is placed on the femur and tibia bones with a polyethylene (plastic) liner between to mimic the old joint and cartilage. The patella may or may not be replaced during surgery as it is dependent on each patient's requirements.
Total knee replacement is proven very effective in improving patient’s pain, allowing return to function and quality of life.
Find out more about
Total Knee Replacement.
Partial (Unicompartmental) Knee Replacement
In some cases, knee osteoarthritis will only affect one compartment of the knee. If indicated, a partial (unicompartmental) knee replacement may be recommended to only replace the damaged area, leaving the other healthy knee compartments maintained. In theory, this can result in a more ‘natural’ feeling knee. After consultation, Dr du Sart will discuss with you if you are a candidate for this surgery.
Find out more about
Partial (Unicompartmental) Knee Replacement.
Knee Arthroscopy
Arthroscopy is not generally recommended to treat osteoarthritis as usually the disease has progressed too far to provide reliable long term results to improve pain. Rather it may be beneficial for patients who are getting symptoms from other areas in their knee as indicated by your Dr du Sart.
Find out more about
Knee Arthroscopy.
Knee Realignment Surgery (Osteotomy)
For patients who are younger with osteoarthritis in one compartment of their knee, this may be an option to improve the alignment of the knee and therefore unload the diseased compartment of the joint. This involves either the tibia (shinbone) or femur (thighbone) being cut and reshaped to help better align the knee joint and relieve pressure on it.
If you are concerned about your knee pain, osteoarthritis or if you require surgery, take the Knee Pain Test today.
1. Felson D, Zhang Y. An update on the epidemiology of knee and hip osteoarthritis with a view to prevention. Arthritis Rheum [Internet]. 1998 Aug [cited 2020 Jun 19]; 41(8):1343–55. Available from: https:// pubmed.ncbi.nlm.nih.gov/9704632/ DOI: 10.1002/1529-0131(199808)41:8<1343::AIDART3>3.0.CO;2-9
2. Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull WHO [Internet]. 2003 Nov 14 [cited 2020 Jun 19]; 81(9):646–56. Available from: https://www. ncbi.nlm.nih.gov/pmc/articles/PMC2572542/ DOI: 10.1590/S0042-96862003000900007

© All rights reserved
For all appointments and enquiries please contact us on:
Phone: 08 9779 9767
Email: admin@ryandusart.com.au
Address: 6 Higgins St, South Bunbury, 6230