HIP
Total Hip Replacement
The total hip replacement is one of the most established, long-lasting, successful surgeries performed today.
It has demonstrated excellent outcomes in relieving pain associated with hip arthritis and the return of a functional pain-free joint allowing patients to return to everyday life.
Procedure
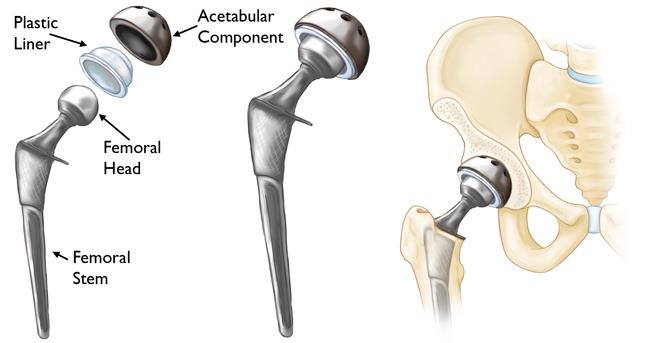
During surgery, the damaged areas are removed and replaced with new components to allow smooth, frictionless movement and restoration of the hip joint. The component options are made of metal, ceramic and/or plastic and are cemented or ‘press fit’ depending on age and quality of bone. At your consultation, Dr du Sart will happily discuss with you the implants and best options.
Once anaesthetised, the hip is dislocated and the damaged femoral head is removed to allow access to the femoral canal. The canal is broached to find a correct fit for the femoral stem replacement. The femoral stem is either cemented or “press fit” into the bone.
The damaged cartilage and osteoarthritic bone of the acetabulum is then reamed to the correct size for the acetabular cup. Screws or cement are sometimes used to hold the cup in place. A polyethylene, ceramic or metal liner is placed into the cup between the femoral head, which is either metal or ceramic, to allow for a smooth gliding surface just like the ball and socket joint of your hip helping return of quality of life.

After Your Operation
Pain Management
Your experience of pain will vary depending on the procedure and the amount of pre-existing damage in the hip. The anaesthetist will discuss the options of pain relief with you. After your operation you will receive pain medication and antibiotics. Once discharged from hospital, you will have the option of pain relief to help with your comfort levels. Usually patients will initially require regular pain relief consisting of paracetamol and anti-inflammatories if indicated. Faster acting pain medication will be given for periods of increased pain during the day (breakthrough pain). Like any medication there can be side effects such as nausea, stomach upset or sedation. However doses can be reviewed to ensure your comfort and reduction of these side effects.
Most patients are pleasantly surprised at how little pain they have after the procedure. A local anaesthetic is injected before and after the procedure to minimise any pain you may feel.
Mobility
Whilst in hospital a physiotherapist will visit you regularly to give you exercises and assist your return to walking. Full weight-bearing and walking is allowed immediately, initially with crutches. Most people are able to walk independently 10-14 days post operation. It is important that you perform the prescribed exercises to ensure optimal recovery.
Return to Work and Sport
Your return to work will vary depending on the procedure and type of work you do. A minimum of 2 weeks off work should be taken to allow for your incision to heal and mobility to improve. For labour intensive work you may require up to 6 weeks before returning to full duties.
During this period patients are not fit to perform duties that include:
- Prolonged standing
- Heavy lifting
- Bending or,
- Excessive stair climbing
Low impact activities such as cycling and swimming/hydrotherapy can be commenced from week 4 and is also recommended to help increase muscle strength and function. High impact activities such as running and jumping are best avoided for 8-12 weeks post operation.
Driving
The Australian Orthopaedic Association (AOA) recommends at least 6 weeks after surgery before you consider recommencing driving. Dr du Sart will be happy to advise you when it is safe to return to driving at his consultation.

© All rights reserved
For all appointments and enquiries please contact us on:
Phone: 08 9779 9767
Email: admin@ryandusart.com.au
Address: 6 Higgins St, South Bunbury, 6230
