KNEE
Partial (Unicompartmental) Knee Replacement
Partial (unicompartmental) knee replacement is a surgery used to replace only the affected area of the knee.
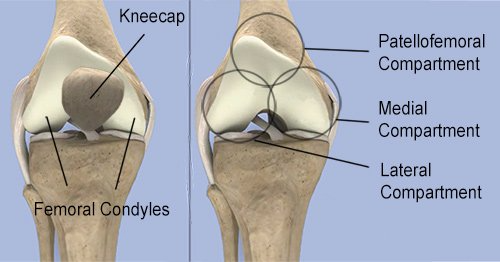
The knee is typically divided into three ‘compartments’, lateral, medial and patellofemoral. In some cases, osteoarthritis will only affect one of the compartments of the knee thus only one compartment requires surgical replacement and the remainder of the joint including the ligaments and tendons are preserved. By doing a partial knee replacement the ‘normal’ movements of the knee are maintained, resulting in a more natural feeling knee.
Benefits
After review and assessment with your medical professionals and Dr du Sart, it will be decided if a partial (unicompartmental) or total knee replacement is best suited for you.
There are a number of reasons why Dr du Sart will recommend a partial (unicompartmental) knee replacement. These include:
- Faster recovery - as more structures of the knee joint, ligaments and tendons are preserved, patients usually spend less time in hospital and can walk earlier as able.
- Smaller incision and less surgical trauma.
- Reduced bleeding.
- Bone conserving - only the affected compartment is operated on.
- More ‘natural’ feeling knee.
- Better movement in the knee.
- Lower complications.
- Partial knee replacements can be revised to total knee replacements if required in the future.
Am I a Candidate?
Patients ideal for partial (unicompartmental) knee replacement are those who have damage localised to one area of the joint, normal ligaments in the knee and minimal deformity or previous trauma to the knee. In cases where arthritis within the knee is too widespread a total knee replacement is considered.
Procedure
Partial (unicompartmental) knee replacement is designed to allow faster return to activity and maintain a ‘natural’ feeling knee.
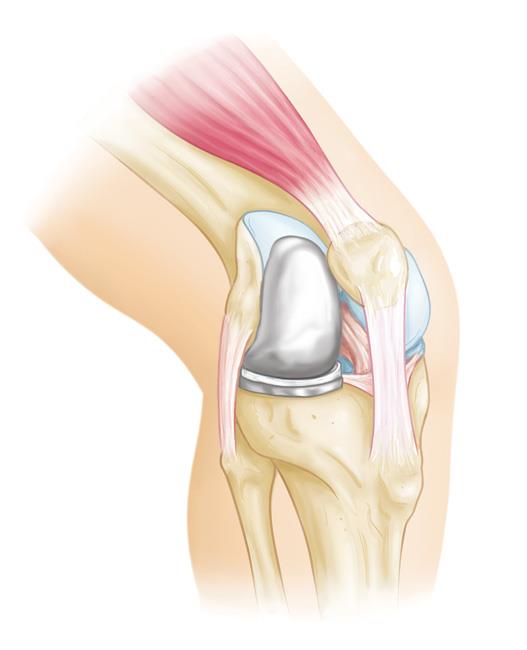
- First a small incision is made to expose the knee joint. The damaged bone and cartilage on the medial or lateral side (or patellofemoral) are removed with specialised cutting jigs and guides.
- Trial components are inserted to check accuracy of cuts and ensure optimal joint alignment
- The definitive components are then inserted with or without cement and the damaged knee is replaced with metal components (tibia and femur) and a plastic bearing between.
After Your Operation
Pain Management
Your pain will vary depending on the individual however most patients find that pain is manageable from the smaller incision and less damaged bone requiring replacing. Usually patients will initially require regular pain relief consisting of paracetamol and anti-inflammatories if indicated. Faster acting pain medication will be given for periods of increased pain during the day (breakthrough pain). Like any medication there can be side effects such as nausea, stomach upset or sedation. However doses can be reviewed to ensure your comfort and reduction of these side effects. It is also recommended to ice and elevate the knee every two hours to help with swelling and pain.

Mobility
Whilst in hospital a physiotherapist will visit you regularly to give you exercises and assist your return to walking. Full weight-bearing and walking is allowed immediately, initially with crutches. Most people are able to walk independently 10-14 days post operation. It is important that you perform the prescribed exercises to ensure optimal recovery.
Management of swelling by regularly applying ice and elevating the knee is also important to reduce swelling and regain movement in the knee.
Return to Work and Sport
Your return to work will vary depending on the procedure and type of work you do. A minimum of 2 weeks off work should be taken to allow for your incision to heal and mobility to improve. For labour intensive work you may require up to 6 weeks before returning to full duties.
During this period patients are not fit to perform duties that include:
- Prolonged standing
- Heavy lifting
- Bending or,
- Excessive stair climbing
Low impact activities such as cycling and swimming/hydrotherapy can be commenced from week 4 and is also recommended to help increase muscle strength and function. High impact activities such as running and jumping are best avoided for 8-12 weeks post operation.
Driving
The Australian Orthopaedic Association (AOA) recommends at least 6 weeks after surgery before you consider recommencing driving. Dr du Sart will be happy to advise you when it is safe to return to driving at his consultation.

© All rights reserved
For all appointments and enquiries please contact us on:
Phone: 08 9779 9767
Email: admin@ryandusart.com.au
Address: 6 Higgins St, South Bunbury, 6230
